The CSA Z8000 Blueprint: What Ontario Medical Clinics Must Know Before Renovating
How Canada’s national healthcare facility standard can save your clinic $50,000+ in failed inspections and change orders
Last Updated: January 16, 2026
Author: Alexey Alexe, RenoEthics Construction
Reading Time: 12 minutes
Dr. Sarah Chen thought she had done everything right. After signing a 5-year lease on a 2,500-square-foot space in Markham for her new family practice clinic, she hired a general contractor with decades of residential experience. The price was competitive—$180 per square foot—and the contractor assured her that “walls are walls” whether in a home or a medical office.
Six months and $450,000 later, Dr. Chen’s dream clinic sat empty, failing its final inspection. The walls between exam rooms barely muffled conversation. The HVAC system couldn’t maintain the air pressure differentials required for her isolation room. The accessible washroom didn’t meet AODA clearances. And the electrical system couldn’t handle the power draw from her diagnostic equipment.
The fix? Another $85,000 in remedial work and a three-month delay—during which she paid rent on a non-operational space while her patient waitlist grew longer.

Dr. Chen’s mistake wasn’t hiring the wrong contractor—it was hiring a contractor who didn’t understand that medical clinics in Ontario aren’t regulated like residential or standard commercial spaces. They’re governed by CSA Z8000, a 500+ page National Standard of Canada that sets forth specific requirements for healthcare facility planning, design, and construction.
If you’re a physician, dentist, physiotherapist, or allied health professional planning to open or renovate a clinic in Ontario, this article will decode CSA Z8000’s requirements in plain language—and show you exactly how to avoid Dr. Chen’s costly mistakes.
What Is CSA Z8000 (and Why Most Contractors Have Never Read It)
CSA Z8000:24, formally titled “Canadian Health Care Facilities – Planning, Design and Construction,” is the third edition of Canada’s national baseline standard for healthcare facility design. Published by CSA Group and developed with financial support from every Canadian province and territory, this standard supersedes previous editions from 2018 and 2011.
Here’s what catches most clinic owners off guard: CSA Z8000 applies to all facilities, public or private, that provide health care treatments, health-related services, or diagnostic testing services regardless of size, location, or range of services. That 1,200-square-foot family practice clinic you’re planning? It falls under the same regulatory framework as a major hospital—just scaled to your scope.
The standard covers a wide range of healthcare facilities including family practice and walk-in clinics, dental and orthodontic offices, physiotherapy and rehabilitation centers, diagnostic imaging facilities, audiology and speech-language pathology clinics, mental health counseling centers, and specialty medical practices like dermatology or cardiology offices.
The standard is built on five core principles, conveniently remembered by the acronym OASIS. These aren’t aspirational goals—they’re enforceable design requirements that building inspectors in Ontario municipalities reference when reviewing medical facility permits.
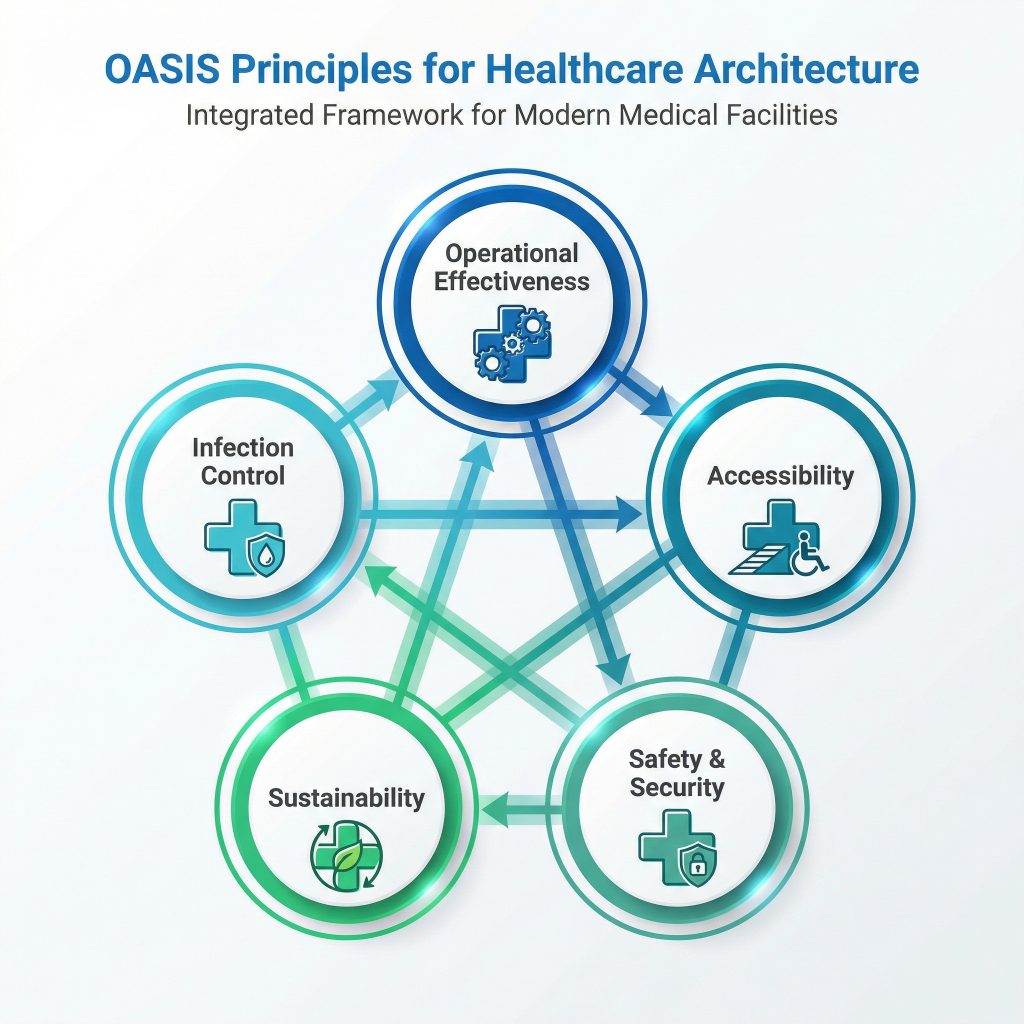
| OASIS Principle | What It Means for Your Clinic |
|---|---|
| Operational Effectiveness | Workflow optimization, staff efficiency, patient throughput |
| Accessibility | AODA compliance plus CSA Z8000 spatial requirements for wheelchair and bariatric patients |
| Safety & Security | Emergency egress, fire safety, medication storage, staff protection |
| Infection Prevention & Control | Hand hygiene stations, HVAC air quality, surface materials, sterilization workflows |
| Sustainability | Energy efficiency, water conservation, climate resilience, lifecycle costs |
The 2024 edition introduced major updates reflecting lessons learned from the COVID-19 pandemic. Enhanced infection prevention and control requirements now address airborne transmission more rigorously. New clauses on climate resilience and business continuity planning help clinics prepare for extreme weather events and operational disruptions. The ambulatory care sections were reorganized specifically for low-acuity community health facilities with high-risk procedures—exactly the type of clinics most family practitioners, dentists, and allied health professionals operate.
Why Your General Contractor Probably Doesn’t Know This Exists
Here’s the uncomfortable truth: CSA Z8000 costs approximately $450 to purchase a single-user digital copy from the CSA Group. Most residential and commercial contractors have never invested in this document because their typical projects don’t require it.

The 2024 edition introduced major updates reflecting lessons learned from the COVID-19 pandemic. Enhanced infection prevention and control requirements now address airborne transmission more rigorously. New clauses on climate resilience and business continuity planning help clinics prepare for extreme weather events and operational disruptions. The ambulatory care sections were reorganized specifically for low-acuity community health facilities with high-risk procedures—exactly the type of clinics most family practitioners, dentists, and allied health professionals operate.
Why Your General Contractor Probably Doesn’t Know This Exists
Here’s the uncomfortable truth: CSA Z8000 costs approximately $450 to purchase a single-user digital copy from the CSA Group. Most residential and commercial contractors have never invested in this document because their typical projects don’t require it.
[IMAGE PLACEHOLDER 3: contractor-reviewing-medical-clinic-blueprints.jpg]
Alt Text: Professional contractor and healthcare facility architect reviewing CSA Z8000 compliant blueprints and building plans for Ontario medical clinic renovation project
When Dr. Chen’s contractor said “walls are walls,” he genuinely believed it. He had successfully renovated 50+ residential basements and 20+ retail stores. But he had never encountered Clause 7.2.4 of CSA Z8000, which specifies minimum sound transmission class (STC) ratings for medical consultation rooms to protect patient confidentiality. He didn’t know that exam rooms require minimum clear floor dimensions of 3.0m × 3.0m (9.8 ft × 9.8 ft) to accommodate wheelchair transfers and medical equipment.
The result? Walls that met residential code (STC-40) but failed healthcare privacy standards (STC-50 minimum, STC-60 preferred). Exam rooms sized for residential bedrooms that couldn’t accommodate a patient in a wheelchair plus an examination table plus the physician. HVAC designed for comfort, not for managing airborne transmission of pathogens.
This is why choosing the right contractor for medical office renovations is critical—it’s not just about construction skills, it’s about regulatory knowledge.
The OASIS Framework: Five Principles That Determine Your Clinic’s Success
Let’s break down each OASIS principle with concrete examples of what it means for your renovation project. This isn’t abstract theory—these are the specific requirements that determine whether your clinic passes inspection or sits empty while you hemorrhage rent money.
Operational Effectiveness: Why Workflow Planning Saves Thousands Monthly
This principle addresses how patients, staff, and materials move through your space. Poor operational design doesn’t just inconvenience people; it costs you money every single day through wasted staff time and reduced patient throughput.
Consider a real case from an Aurora dental practice. The clinic was renovated without considering sterilization workflow. The result? Dental assistants walked 127 steps per patient cycle transporting instruments between operatories and the sterilization room. Over 25 patients per day, this added 90+ minutes of wasted motion—time that could have been spent on patient care or additional appointments.
CSA Z8000’s operational effectiveness requirements address these issues systematically. The standard mandates separation of “clean” and “dirty” workflows to prevent cross-contamination. Hand hygiene stations must be positioned within 2 steps of patient care areas—not down the hall or in a shared washroom. Storage should be positioned to minimize staff travel distance, and patient flow should prevent backtracking through waiting areas.
The cost impact is stark. Fixing workflow issues post-construction requires relocating plumbing, HVAC, and electrical—typically $15,000-$40,000. Planning workflow correctly during the design phase costs nothing extra. You’re going to build walls and install sinks anyway; putting them in the right locations is simply a matter of forethought.
Accessibility: Beyond Door Widths and Ramps
When most people hear “accessibility,” they think of AODA-compliant door widths and wheelchair ramps. CSA Z8000 goes significantly further, mandating specific spatial requirements for wheelchair maneuverability, patient transfer, and bariatric patient accommodation that many contractors overlook.

The standard requires minimum clear floor space of 1,500mm × 1,500mm (59″ × 59″) adjacent to exam tables for wheelchair turning radius. Door widths must provide 915mm (36″) clear opening—that’s the actual passage width when the door is open, not just the door leaf width. Accessible washrooms need a full 1,700mm × 1,700mm (67″ × 67″) turning circle. Examination tables should be height-adjustable, lowering to 48cm (19″) to enable safe patient transfers. Patient corridors must be at least 2,400mm (94″) wide to allow two wheelchairs to pass each other.
A Richmond Hill physiotherapy clinic learned these requirements the hard way. They designed their space with standard commercial 32″ doors and 900mm corridors, assuming this met accessibility codes. During their first month of operation, they discovered that bariatric wheelchairs couldn’t navigate to treatment rooms. The clinic lost 15% of potential patients who required accessibility accommodations. Retrofitting doors and corridors cost $22,000—money that could have been saved with proper planning.
Our comprehensive guide on AODA compliance for medical clinics explores these requirements in greater detail.
Safety & Security: Protecting Patients and Staff
This principle encompasses physical safety (slip-resistant flooring, emergency egress), patient security (controlled access to medication storage), and staff safety (panic buttons, secure parking visibility). While it might seem straightforward, safety requirements in healthcare settings are more complex than standard commercial spaces.
Emergency egress routes from all patient care areas must remain unobstructed at all times—no temporary storage, no equipment staging. Walls separating your clinic from adjacent commercial tenants must meet fire-resistance ratings, typically 1-hour in Ontario. If you’re using oxygen or nitrous oxide for sedation, your piped gas systems must meet CSA Z305.6 standard for medical gas installations. Secure medication storage requires lockable cabinets or rooms meeting federal regulations for controlled substances.
A Vaughan dental office discovered the consequences of overlooking medical gas standards when they installed nitrous oxide sedation equipment without consulting an engineer familiar with these requirements. During the fire inspection, the Fire Marshal red-tagged the entire clinic because the gas lines lacked proper seismic bracing, emergency shutoffs, and alarm systems. Bringing the system into compliance cost $18,000 and delayed their opening by six weeks.
Infection Prevention & Control: The Post-COVID Priority
Post-COVID, infection prevention and control has become the most scrutinized aspect of medical facility design. CSA Z8000:24 significantly expanded IPC requirements to reflect current evidence on airborne transmission, surface contamination, and healthcare-associated infections (HAIs).
Hand hygiene stations must be positioned within 5 meters of every patient care area, with hands-free operation through foot pedals or automatic sensors. Your HVAC system needs to provide a minimum of 6 air changes per hour (ACH) in exam rooms and 12+ ACH in isolation rooms. Speaking of isolation rooms, they must maintain negative pressure (-2.5 Pa minimum) relative to corridors to prevent airborne pathogen spread.
Surface materials matter more than aesthetics. All patient care areas require non-porous, cleanable finishes—that means no carpet, unsealed wood, or fabric-covered furniture. The sterilization room needs physical separation between contaminated instrument processing areas and clean storage areas to prevent cross-contamination.
Common failures we see include inadequate handwashing stations (a Newmarket walk-in clinic had only two sinks for eight exam rooms, forcing staff to leave patient areas to wash hands), poor HVAC design (a Bradford family practice installed a residential-grade system that couldn’t provide adequate air changes, leading to persistent odors and failed health inspections), and inappropriate flooring choices (carpet in waiting areas may be aesthetically pleasing, but it’s difficult to sanitize and harbors pathogens).
The fix cost for these mistakes is substantial. Retrofitting proper ventilation after construction typically runs $25,000-$75,000, including new air handling units, ductwork, and commissioning testing. Installing it correctly during construction adds only $8,000-$15,000 to your HVAC budget. For detailed guidance on this topic, see our article on choosing the right materials for infection control.
Sustainability: Long-Term Operational Savings
The 2024 edition of CSA Z8000 added new clauses addressing climate resilience, energy management, and sustainable healthcare facility operations. This isn’t just about environmental responsibility—it’s about long-term operational costs that directly impact your bottom line.
Sustainability requirements include energy-efficient HVAC systems with heat recovery where feasible, LED lighting with occupancy sensors to reduce energy consumption, water conservation through low-flow fixtures in all washrooms and clinical sinks, durable low-maintenance materials that reduce lifecycle replacement costs, and climate resilience planning including backup power for critical systems.
The return on investment is compelling. A 2,500-square-foot clinic in Barrie invested an additional $12,000 in LED lighting with smart controls, high-efficiency HVAC, and low-flow fixtures. Their annual utility savings: $3,400. Payback period: 3.5 years. Over a 10-year lease, total savings exceed $34,000—nearly three times their initial investment.
The Three Most Expensive CSA Z8000 Compliance Failures
After consulting on numerous medical facility projects across Ontario, three mistakes consistently generate the highest remediation costs. Understanding these failure modes can save you tens of thousands of dollars—and months of delays.
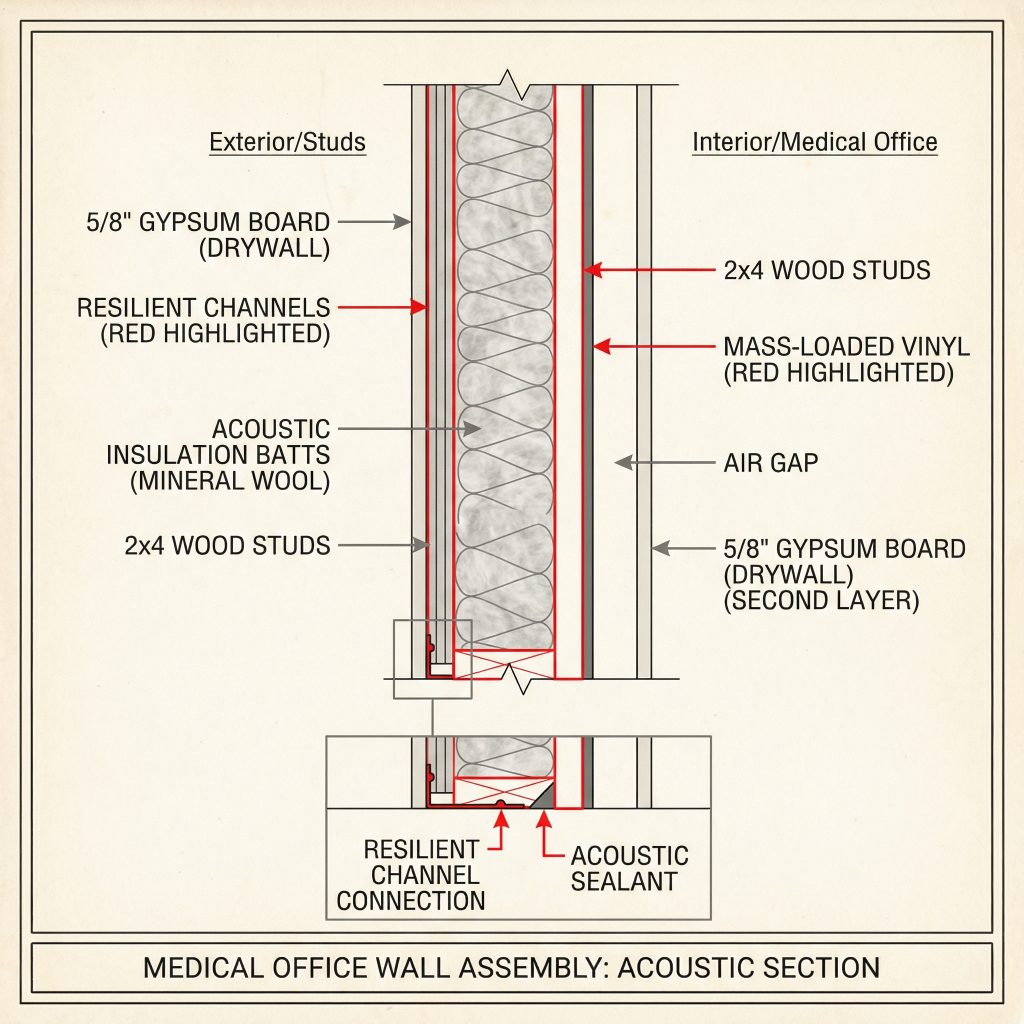
Mistake #1: Inadequate Acoustic Privacy ($25,000-$75,000 to Fix)
Patient-physician conversations are protected health information under PHIPA (Personal Health Information Protection Act). If someone in the waiting room can overhear an exam room discussion, you’re not just failing CSA Z8000—you’re legally non-compliant with provincial privacy legislation.

CSA Z8000 requires walls between exam rooms and public areas to achieve STC-50 minimum (STC-60 preferred) to ensure speech privacy. Understanding what these ratings mean is crucial for making informed decisions about your construction.
| STC Rating | What You'll Hear | Suitability for Medical Use |
|---|---|---|
| STC-40 | Loud speech is audible and understandable | Typical residential wall—NOT acceptable for medical clinics |
| STC-50 | Loud speech is audible but not intelligible | Minimum standard for medical facilities |
| STC-60 | Normal speech is inaudible | Best practice for healthcare—recommended for all exam rooms |
Achieving STC-60 requires a methodical approach combining three acoustic principles: mass, decoupling, and absorption. For mass, you need 5/8″ Type-X drywall on both sides of the wall—not standard 1/2″ drywall that most contractors default to. For decoupling, install resilient channels or use staggered stud construction to prevent sound transmission through the framing. For absorption, fill the wall cavity with acoustic insulation rated at R-12 minimum. Finally, seal all penetrations—electrical boxes, HVAC ducts, door frames—with acoustic caulk, because sound will find and exploit even the smallest gaps.
A specialty cardiology clinic in Markham discovered during their first week of operation that conversations in Exam Room 1 were clearly audible in the waiting room. The contractor had used standard residential framing with 1/2″ drywall, assuming commercial code was sufficient. Remediation required demolishing and rebuilding five exam room walls, relocating electrical and data cabling, and repainting the entire clinic due to dust contamination. The clinic closed for two weeks during construction. Total cost: $68,000. The cost to build it correctly from the start: $5,500.
Mistake #2: Non-Compliant HVAC Systems ($50,000-$200,000 to Fix)
Medical clinics require specialized HVAC systems that maintain specific air quality, temperature, humidity, and pressure differentials. Residential or standard commercial HVAC cannot meet these requirements—full stop. This isn’t about comfort; it’s about infection control and regulatory compliance.
CSA Z8000’s HVAC requirements (aligned with CSA Z317.2 standard for healthcare facilities) specify minimum 6 air changes per hour in exam rooms and 12 ACH in isolation rooms. Filtration must be MERV-13 minimum (MERV-15 for isolation rooms) to capture airborne pathogens. Isolation rooms must maintain negative pressure while sterile procedure rooms require positive pressure. Temperature control must maintain 20-24°C (68-75°F) year-round, and humidity must remain between 30-60% to prevent mold growth and maintain equipment function.
Common HVAC failures follow predictable patterns. A 3,000-square-foot clinic in Aurora installed a residential furnace sized by square footage alone, not accounting for the higher air change requirements. The system ran continuously but couldn’t maintain temperature or air quality. Replacement cost: $45,000. A multi-specialty clinic installed a single-zone system; when radiology needed cooling for heat-generating imaging equipment, exam rooms became frigid. Installing zone controls post-construction: $18,000. A dental practice recirculated 100% indoor air without outside air makeup, causing CO2 buildup and odor problems. Adding outside air supply and properly sizing equipment: $32,000.
The prevention strategy is straightforward but non-negotiable: hire a mechanical engineer experienced in healthcare facilities—not just commercial buildings. Budget 15-20% more for HVAC than standard commercial construction. The premium is approximately $8-15 per square foot, but it’s not optional for compliance.
Mistake #3: Improper Medical Equipment Integration ($15,000-$50,000 to Fix)
Medical equipment has specialized electrical, plumbing, data, and structural requirements that must be planned from day one. The “we’ll figure it out when the equipment arrives” approach is a recipe for expensive disasters.
A diagnostic imaging clinic in Richmond Hill completed construction before confirming their X-ray machine specifications. When the equipment finally arrived, they discovered the machine weighed 2,400 pounds while floors were only rated for 50 pounds per square foot. The power requirement was 480V three-phase—the building only had 208V. Lead-lined walls required for radiation safety weren’t installed. The equipment dimensions didn’t fit through doorways.
Remediation included structural floor reinforcement with steel beams, electrical service upgrade and transformer installation, lead-lining walls after construction (requiring removal and reinstallation of finished drywall), and widening two doorways. Total cost: $127,000. Project delay: 4 months.
Prevention requires discipline and early planning. Finalize equipment selection before finalizing architectural plans. Obtain “cut sheets” (specification documents) from equipment vendors showing exact dimensions, weight, power, plumbing, and data requirements. Engage an electrical engineer to verify power capacity for all medical devices—diagnostic equipment often requires dedicated circuits. Plan equipment delivery and installation routes by measuring doorways, corridors, and elevators to ensure equipment can physically reach its destination. Consider future expansion by installing additional electrical capacity and data drops for equipment you may add in years 2-5.
The Pre-Construction Compliance Checklist
Before signing any construction contract for your medical office renovation, you need to ask specific CSA Z8000-related questions. If your contractor can’t answer them confidently—or dismisses them as “overthinking”—that’s a massive red flag.

Essential Questions to Ask Your Contractor
About CSA Z8000 Knowledge:
Start with the basics: “Have you renovated medical facilities in Ontario before? Can you provide three references?” Follow up with “Are you familiar with CSA Z8000 and CSA Z317.13 (infection control during construction)?” Finally, confirm insurance: “Do you have professional liability insurance with minimum $2 million coverage?”
About HVAC:
HVAC is where most failures occur, so probe deeply. “Will you engage a mechanical engineer who specializes in healthcare HVAC systems?” Ask specifically, “How will you ensure the HVAC system meets CSA Z317.2 requirements for air changes per hour?” Confirm filtration: “Will the system include MERV-13 or higher filtration?” If your clinic needs isolation capacity, ask: “If we need an isolation room, can you design and install negative pressure?”
About Acoustics:
Speech privacy is non-negotiable. “What STC rating will walls between exam rooms achieve?” The answer should be STC-50 minimum, STC-60 preferred. Ask about comprehensive soundproofing: “How will you prevent sound transmission through ceiling plenums and electrical penetrations?” Request verification: “Will you provide acoustical testing after construction to verify sound attenuation?”
About Infection Control:
Get specific about IPAC compliance. “How many hand hygiene stations will be installed, and where?” There should be stations within 5 meters of every patient care area. “What flooring materials do you recommend for patient care areas?” The correct answer involves non-porous, seamless materials. “How will you contain dust and debris during construction to prevent contamination?”
About Accessibility:
“Have you designed spaces to meet both AODA and CSA Z8000 accessibility requirements?” Note the distinction—both are required. “What are the clear floor dimensions in exam rooms to accommodate wheelchairs?” The answer should reference the 3.0m × 3.0m (9.8 ft × 9.8 ft) minimum.
About Project Management:
Financial planning for medical projects differs from residential or commercial work. “What is your typical contingency percentage for medical facility projects?” The correct answer is 15-20%, not the 10% typical for residential work. “How will you coordinate with medical equipment vendors for installation requirements?” “What is the timeline for permit approval, and have you accounted for municipal review delays?”
Red Flags That Should End the Conversation
Some warning signs are absolute deal-breakers. If your contractor dismisses your questions as “overthinking” or “over-engineering,” walk away. If they suggest “we’ll figure it out during construction,” run. If they have only residential or retail experience with no healthcare portfolio, they’re not qualified. If they propose “value engineering” (cutting costs) on HVAC, acoustic, or accessibility features, they don’t understand healthcare compliance. If they don’t mention hiring specialized consultants like mechanical engineers or acoustic consultants, they’re operating outside their depth.
The True Cost of CSA Z8000 Compliance
Let’s address the question every clinic owner asks: “How much more does it cost to build a CSA Z8000-compliant facility versus a standard commercial space?” The answer requires breaking down both upfront costs and the potential cost of non-compliance. When you compare these numbers honestly, the value proposition becomes clear.
Realistic Budget Comparison for 2,500 Square Foot GTA Clinic
| Construction Element | Standard Commercial | CSA Z8000-Compliant | Premium Cost |
|---|---|---|---|
| Base construction (@$180 vs @$210/sq ft) | $450,000 | $525,000 | +$75,000 |
| HVAC system upgrade | Included | +$18,000 | +$18,000 |
| Acoustic walls (STC-40 vs STC-60) | Basic | Enhanced | +$12,000 |
| Accessibility features | AODA minimum | Full CSA Z8000 | +$8,000 |
| Hand hygiene stations (2 vs 6) | $3,000 | $10,500 | +$7,500 |
| Professional fees (engineers, consultants) | $15,000 | $28,000 | +$13,000 |
| Total Project Cost | $468,000 | $608,500 | +$140,500 |
| Cost per Square Foot | $187/sq ft | $243/sq ft | +$56/sq ft |
That’s a 30% increase in construction costs. Before you recoil at the premium, let’s look at what non-compliance actually costs when inspections fail and remediation begins.
The Financial Reality of Non-Compliance
| Compliance Issue | Remediation Cost | Timeline Impact |
|---|---|---|
| Failed acoustic inspection | $25,000-$75,000 | 2-4 weeks delay |
| HVAC system replacement | $45,000-$80,000 | 3-6 weeks delay |
| Accessibility violations | $15,000-$30,000 | 2-3 weeks delay |
| IPAC non-compliance | $20,000-$50,000 | 1-4 weeks delay |
| Potential Total | $105,000-$235,000 | 8-17 weeks delay |
But remediation costs are only part of the financial damage. During those 8-17 weeks of delay, you’re paying rent on a non-operational space ($6,000-$10,000/month). If you’re an established practice relocating, you’re losing patient revenue ($30,000-$60,000/month). You’re paying staff salaries while the clinic sits closed ($15,000-$25,000/month). And you’re suffering reputation damage and patient attrition that’s difficult to quantify but very real.
The total financial impact of non-compliance: $156,000-$400,000 or more. Suddenly, that $140,500 compliance premium looks like the bargain it is. For a detailed analysis of medical office renovation costs, see our comprehensive guide on how much it costs to renovate a medical office in Ontario.
Municipal Variations Across the GTA
While CSA Z8000 is a national standard, municipalities retain discretion in how they enforce it and what additional requirements they layer on top. Understanding these local variations helps you set realistic timelines and budgets for your project.
Toronto: Comprehensive Review with Green Standards
Toronto’s building department conducts thorough reviews that take 4-6 weeks for straightforward medical clinic renovations, extending to 8-12 weeks for complex projects. The city has additional Green Standard requirements for energy efficiency that go beyond CSA Z8000’s sustainability provisions. Permit fees are calculated as a percentage of construction value (approximately 1.1%) plus per-square-foot charges. For a 2,500 square foot clinic with $500,000 construction value, expect $7,000-$9,000 in permit fees.
Markham: Strict Accessibility Enforcement
Markham generally processes permits faster than Toronto—3-5 weeks is typical. However, the building department enforces accessibility standards strictly and has detailed parking and loading requirements that can catch applicants off guard. Permit fees use a similar percentage-based model to Toronto. Markham Building Department offers a specific pre-consultation process for medical facilities that we strongly recommend using—it can identify potential issues before formal submission.
Barrie: Faster Processing with Fire Safety Focus
Barrie typically processes medical facility permits in 2-4 weeks, making it the fastest of these three municipalities. The building department places additional scrutiny on fire safety, particularly in older buildings. Permit fees are lower than Toronto or Markham—approximately $5,000-$7,000 for the same project that would cost $7,000-$9,000 in Toronto. The smaller building department provides more personalized service, which can be an advantage when navigating complex healthcare requirements.
For projects spanning multiple municipalities, engaging a permit expediter familiar with local building departments makes sense. Their fees ($3,000-$8,000) are typically offset by time savings and reduced risk of resubmissions that delay your project.
Your Implementation Roadmap: From Planning to Opening
If you’re serious about opening a medical clinic in Ontario that passes inspection the first time, here’s your month-by-month implementation roadmap. This timeline assumes a 2,000-3,000 square foot clinic in the Greater Toronto Area.
Phase 1: Assemble Your Team (Months 1-2)
Your professional team determines project success more than any other factor. You need a healthcare-specialized architect (BCIN or OAA registered) with a medical facility portfolio you can review. Hire a mechanical engineer familiar with CSA Z317.2 for healthcare HVAC design. Engage an electrical engineer experienced with medical equipment power requirements—this isn’t standard commercial electrical work. Select a general contractor with healthcare construction experience and demonstrable CSA Z8000 knowledge. For clinics requiring speech privacy (most medical practices), hire an acoustic consultant.
Budget $28,000-$70,000 for this professional team depending on your project’s complexity. This seems expensive until you remember that skipping these specialists can cost you $100,000-$400,000 in remediation.
Phase 2: Pre-Construction Planning (Months 2-4)
During this phase, your team produces detailed architectural drawings showing all CSA Z8000-compliant features, mechanical drawings with air change per hour calculations for each room, electrical one-line diagrams showing dedicated circuits for medical equipment, acoustic specifications and wall assembly details, and an IPAC protocol for the construction phase. This documentation forms the foundation of your permit application.
Phase 3: Permitting (Months 4-5)
Design review and permit drawing preparation typically takes 3-4 weeks. Municipal plan review varies by location—2-6 weeks depending on the municipality and current workload. If revisions are required, add 1-2 weeks for resubmission. Permit issuance follows 1-2 weeks after approval. Request a pre-submission meeting with your municipal building department. Many offer free consultations where you can identify potential issues before formal submission, potentially saving weeks on the back end.
Phase 4: Construction (Months 6-9)
Your inspection schedule will include foundation inspection (if applicable), framing inspection (before drywall installation), HVAC rough-in inspection, plumbing rough-in inspection, electrical rough-in inspection, fire safety inspection, final building inspection, and final occupancy inspection. Each failed inspection adds 1-2 weeks to your timeline while issues are corrected and re-inspection is scheduled. A typical 2,000-3,000 square foot clinic takes 3-6 months for construction if planned properly.
Phase 5: Commissioning & Opening (Months 9-10)
Before your first patient walks through the door, complete HVAC system commissioning to verify air change rates and pressure differentials. Conduct acoustic testing to verify STC ratings actually meet specifications. Perform an accessibility audit to confirm compliance. Complete final cleaning following IPAC protocols. Orient your staff to facility features and workflows. Install and test all medical equipment. Consider a soft opening with a limited patient schedule to identify operational issues while the stakes are low.
Frequently Asked Questions About CSA Z8000 Compliance
After working with dozens of healthcare professionals planning clinic renovations, we hear the same questions repeatedly. Here are the answers to the most common concerns about CSA Z8000 compliance and medical facility construction in Ontario.
What is CSA Z8000 and why does it matter for medical clinic renovations?
CSA Z8000 is Canada’s national standard for healthcare facility planning, design, and construction. It applies to all medical facilities in Ontario, public or private, regardless of size. The standard sets specific requirements for acoustic privacy, HVAC systems, accessibility, infection control, and safety that go beyond standard commercial building codes.
It matters because your building inspector will reference this standard during permit review and final inspections. Non-compliance can result in failed inspections, costly remediation ($50,000-$200,000+), and delayed openings. Even a small family practice clinic with three exam rooms falls under this standard’s jurisdiction.
How much more does CSA Z8000-compliant construction cost?
CSA Z8000-compliant construction typically costs $50-60 per square foot more than standard commercial construction. For a 2,500 square foot clinic, this represents approximately $125,000-$150,000 in additional upfront costs.
However, this premium is far less expensive than remediation after failed inspections, which can cost $100,000-$400,000 or more when you factor in construction fixes, rent on non-operational space, lost revenue, and timeline delays. The compliance premium is essentially insurance against much larger costs down the road.
What are the OASIS principles in CSA Z8000?
OASIS stands for the five core principles that guide healthcare facility design:
- Operational effectiveness and efficiency – workflow optimization and staff productivity
- Accessibility – AODA compliance plus enhanced spatial requirements for wheelchairs and bariatric patients
- Safety and security – emergency egress, fire safety, medication storage, staff protection
- Infection prevention and control – hand hygiene stations, HVAC air quality, surface materials, sterilization protocols
- Sustainability – energy efficiency, water conservation, climate resilience, lifecycle costs
These aren’t aspirational guidelines—they’re enforceable requirements that building inspectors reference during permit reviews and final inspections. Every design decision in your clinic should be evaluated against these five principles.
Do general contractors need specialized training for medical facility construction?
Yes, absolutely. Medical facility construction requires specialized knowledge of CSA Z8000, CSA Z317.2 (HVAC for healthcare), CSA Z317.13 (infection control during construction), and healthcare-specific building codes. This knowledge doesn’t come from residential or standard commercial construction experience.
General contractors without healthcare experience often miss critical requirements for acoustic privacy (STC ratings), air quality (air changes per hour), infection control (hand hygiene station placement), and accessibility (wheelchair turning radiuses). These oversights lead to failed inspections and costly remediation that can exceed $100,000.
When interviewing contractors, ask specifically about their healthcare portfolio and familiarity with CSA Z8000. If they can’t discuss OASIS principles or HVAC air change requirements confidently, they’re not qualified for medical facility work.
How long does it take to get a building permit for a medical clinic in Ontario?
Permit timelines vary significantly by municipality. In Toronto, expect 4-6 weeks for straightforward renovations and 8-12 weeks for complex projects. Markham typically processes permits in 3-5 weeks. Barrie is fastest at 2-4 weeks.
These timelines assume your application is complete and compliant. Incomplete applications or designs that don’t meet CSA Z8000 requirements can add 2-4 weeks for revisions and resubmission. This is why pre-submission meetings with your building department are so valuable—they can identify potential issues before you formally apply.
Can I renovate my medical clinic while it’s still operating?
Yes, but it requires careful planning and strict infection control protocols. Phased construction allows you to renovate sections of your clinic while maintaining operations in other areas. This approach minimizes revenue loss but extends your overall timeline and requires additional dust containment, noise control, and IPAC measures.
The key is maintaining separate zones—active patient care areas must be completely isolated from construction zones. This typically adds 15-20% to your construction costs but can save tens of thousands in lost revenue if your practice would otherwise close completely. See our guide on designing patient-friendly waiting areas for strategies to minimize disruption during renovations.
What happens if my clinic fails its final inspection?
If your clinic fails final inspection, you cannot legally open for business until violations are corrected and the space passes re-inspection. The building department will issue a deficiency list specifying what must be fixed. Common failures include inadequate acoustic privacy, HVAC systems not meeting air change requirements, accessibility violations, or missing IPAC features.
Remediation costs vary by issue severity but typically range from $25,000-$75,000 for acoustic problems, $50,000-$200,000 for HVAC system replacement, and $15,000-$50,000 for accessibility or infection control violations. Re-inspection scheduling adds 1-2 weeks to your timeline for each failed inspection.
This is why working with healthcare-specialized contractors from the beginning is so critical—they build it right the first time, avoiding these costly failures entirely.
Does CSA Z8000 apply to dental offices, physiotherapy clinics, and other allied health facilities?
Yes. CSA Z8000 applies to all healthcare facilities in Ontario, regardless of the type of care provided. This includes dental offices, physiotherapy clinics, chiropractic practices, audiology clinics, massage therapy clinics, mental health counseling centers, and any other facility providing health-related services or diagnostic testing.
Each specialty has additional requirements beyond the base CSA Z8000 standard. For example, dental offices need specialized plumbing for suction systems and amalgam separators. Diagnostic imaging clinics require lead-lined walls and specific electrical configurations. Audiology clinics need enhanced acoustic isolation. Your contractor and design team should understand both the general CSA Z8000 requirements and the specialty-specific needs of your practice type.
For specialty-specific guidance, see our articles on audiology clinic transformations and veterinary clinic renovations (which share similar infection control and workflow requirements).
Conclusion: Your Blueprint for Success
Dr. Chen’s story from the opening of this article has a happy ending. After the $85,000 in remedial work and three-month delay, her clinic finally opened. Today, it’s a thriving practice with 2,800 active patients. But she admits that if she had to do it over again, she would have hired a contractor who spoke fluent CSA Z8000 from day one. The stress, financial strain, and professional uncertainty during those three months of delay were far more costly than any upfront premium for proper planning.
The lessons are clear and unambiguous. CSA Z8000 compliance isn’t optional—it’s the regulatory framework that governs medical facility construction in Ontario. The upfront premium for compliance (approximately $50-60 per square foot) is far less expensive than the cost of remediation ($100-250 per square foot). Not all contractors are qualified to build medical facilities—healthcare construction is a specialized discipline requiring specific knowledge that most general contractors simply don’t possess. Your team matters more than your budget when it comes to avoiding costly mistakes. And here’s the good news: planning for compliance from day one costs nothing extra—you’re going to build walls and install systems anyway; doing it right the first time is simply a matter of knowledge and forethought.
If you’re planning to open or renovate a medical clinic anywhere in the Greater Toronto Area—from Barrie to Aurora, Markham to Richmond Hill—RenoEthics Construction brings specialized expertise in CSA Z8000-compliant healthcare facility renovation. Whether you’re opening a family practice, walk-in clinic, or pharmacy, we’ve invested in the training, consultants, and documentation systems to ensure your clinic passes inspection the first time.
Because in healthcare construction, there’s no such thing as a “good enough” solution. There’s only code-compliant—or closed by the building inspector.
About the Author
Alexey Alekseev is the founder of RenoEthics Construction, specializing in medical facility renovations across Ontario’s Greater Toronto Area. With expertise in CSA Z8000 compliance, IPAC protocols, and healthcare-specific construction challenges, RenoEthics has helped dozens of healthcare professionals open code-compliant, patient-centered clinics without costly delays or change orders.
Need help with your medical clinic renovation? Contact RenoEthics for a complimentary CSA Z8000 compliance assessment of your project plans.
Related Resources from RenoEthics
- Permits and Regulations for Medical Renovations in Ontario
- Choosing the Right Materials for Infection Control in Healthcare Settings
- Understanding AODA Compliance for Medical Clinics in Ontario
- How Much Does It Cost to Renovate a Medical Office in Ontario?
- What to Look for in a Medical Office Renovation Contractor
- How to Plan a Medical Office Renovation in Ontario: Step-by-Step Guide